- IVF and Female Infertility: Causes, Diagnosis, and Treatment
- IVF Success Rates by Age, Diagnosis, and Additional Treatments
- Comprehensive Guide to IVF Treatment in Turkey: Cost, Planning, Experience
- How To Prepare For IVF: Diet, Exercise, And Lifestyle Guide For IVF Success
- After IVF: Implantation, the 2-Week Wait, and Failure
In the previous chapter, we discussed female infertility and how IVF can help with that. Now we will take a look at male infertility and its treatments. Over the last few years, male infertility has become more common. Generally, when a couple seeks treatment for infertility, the first things doctors look at are the female factors, but now it’s estimated that the male factor contribution to infertility is somewhere between 20% to 70% for couples seeking treatment. To understand how male fertility works, we will take a look at;
- Male reproductive system and how it works,
- The Causes of infertility in men,
- How semen analysis can diagnose these problems,
- How IVF treats male infertility,
- What procedures are used in conjunction with IVF to treat male infertility.
What's the male reproductive system and how does it work?
To properly understand how IVF can treat male fertility, we will begin by learning about the male reproductive system and the purpose of each organ. Then we will move on to how sperm production works.
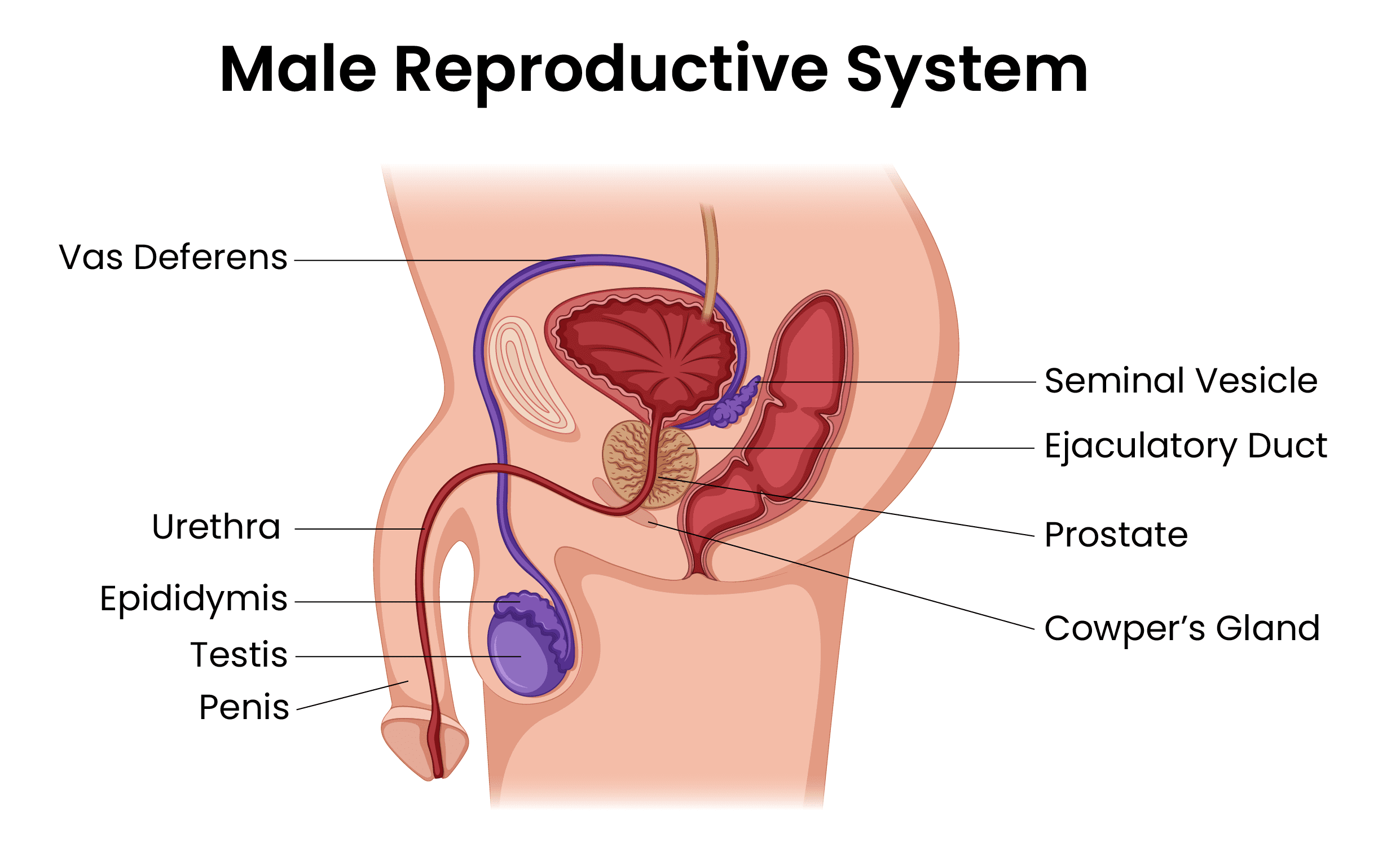
- Testes: Testes (testicles) reside in the scrotum, and this is where testosterone is produced. Inside the testes, there are microscopic tubes (seminiferous tubules) where sperm production (spermatogenesis) happens. Most men are born with 2 testes in their scrotum, but some men can have undescended testes.
- Epididymis: Epididymis is a tubular structure that sits on top of each testis. During spermiogenesis, the cells that start to grow in the testicles reach their maturity in the epididymis and acquire motility.
- Vas deferens: Vas deferens is the tube that connects the epididymis to the urethra, where semen will be ejaculated out of the body.
- Seminal vesicle: Seminal vesicles are glands that are connected to vas deferens. Their role is to produce a nutrient-rich fluid so the spermatozoa can survive.
- Ejaculatory duct: Ejaculatory duct is where vas deferens and the seminal vesicles connect.
- Cowper’s gland: Also known as bulbourethral glands, they are located next to the urethra and the prostate gland. The purpose if it is to produce a fluid that will neutralize the pH in the urethra between the discharge of urine and the semen.
- Prostate: The prostate is also like the seminal vesicle in its purpose, it produces fluids to help the spermatozoa survive.
- Urethra: Urethra runs through the middle of the penis, and it’s where both urine and semen leave the body.
- Penis: The penis is the male sex organ. The urethra opens up from the penis and allows for the discharge of semen and urine.
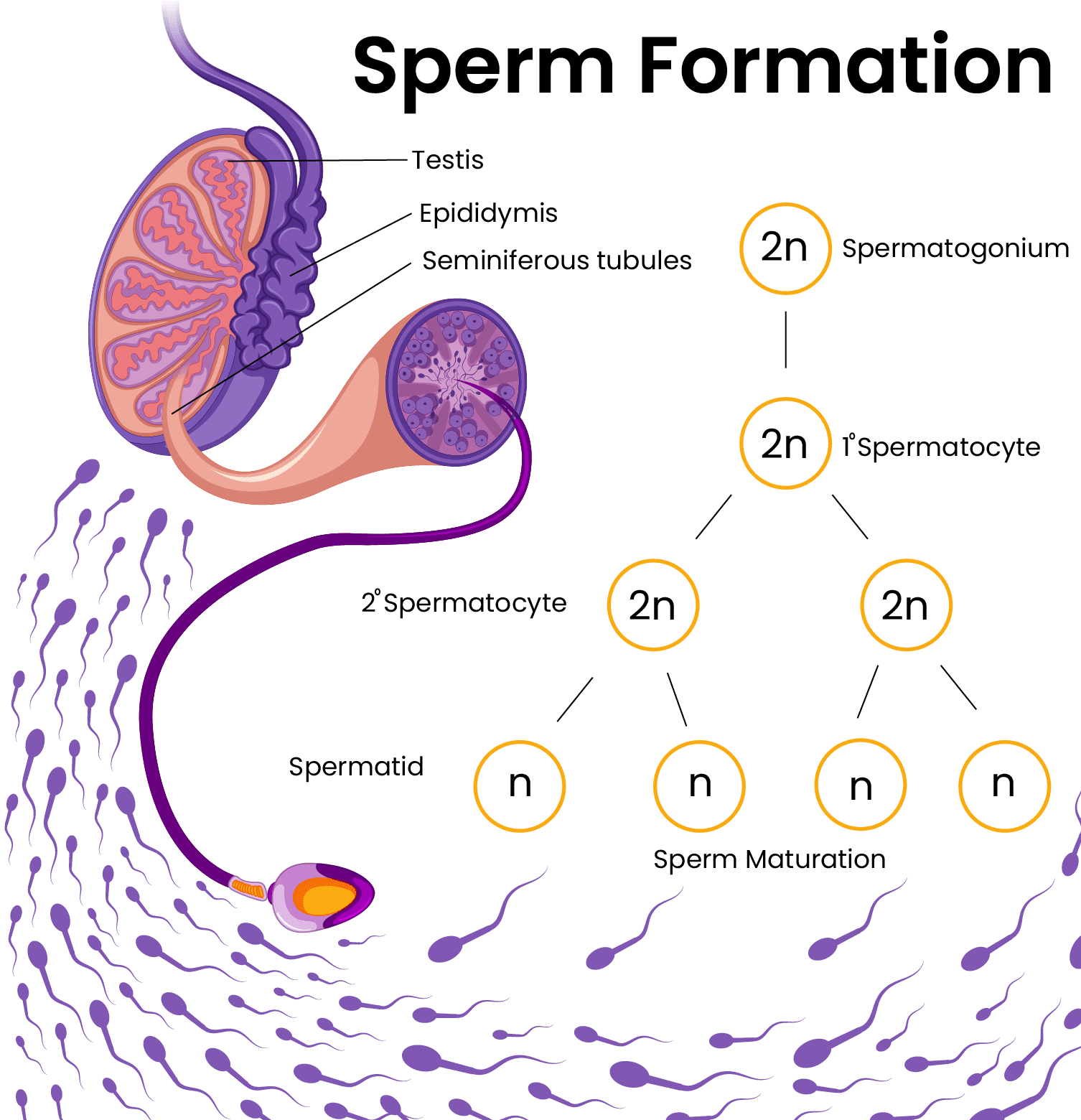
How is sperm produced?
Sperm production starts with the germ cells. All male children are born with millions of germ cells in the seminiferous tubules in their testes. As the male child reaches puberty, multiple hormones are secreted by the brain that helps develop the sex organs and support the production of sperm.
The difference between female egg production and sperm production is that in females one germ cell will produce one egg, but the male germ cell will produce multiple sperm cells. While females can produce eggs for a certain amount of time, men can produce sperm cells until they die, but the number and the quality decline with age.
Immature sperm cells divide multiple times to reach maturity (spermatogenesis). However, they’re not ‘motile’ meaning they're not moving. They’ll acquire motility in the epididymis. And during intercourse, the epididymis and the other parts of the male reproductive system will contract and release semen into the female reproductive tract.
What causes male infertility?
Male infertility is just as complex as female fertility. Multiple factors play a role, such as; hormonal problems, problems with the formation of the reproductive organs, problems with the sperm production itself, etc. Let’s go over these factors in detail.
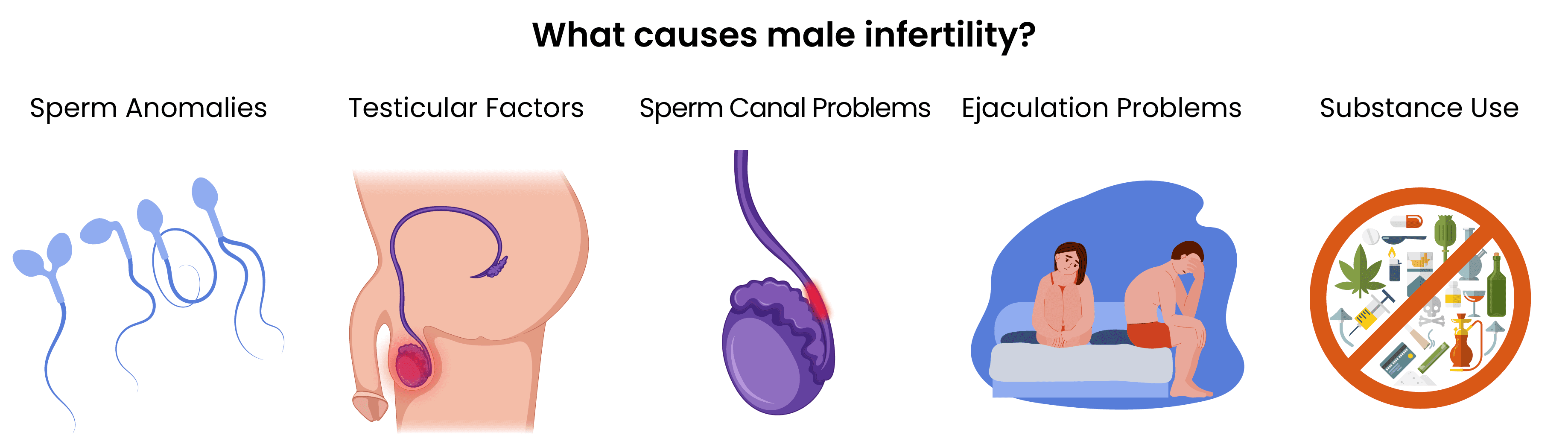
Sperm Anomalies
Most cases of male infertility are due to some abnormality with the sperm cells. For fertilization to occur, there should be enough spermatozoa in the semen, with healthy patterns of movement and normal formation. Sperm quality is directly related to spermatogenesis, the formation of the male reproductive system, and lifestyle factors. If there is any problem with these factors, male infertility is a possibility. Some of the sperm quality problems are as follows:
- Azoospermia is the absence of sperm in the semen. Azoospermia is classified into two groups. Obstructive Azoospermia is when the absence of spermatozoa is caused by a defect in the reproductive tract, but there is spermatogenesis. Non-obstructive Azoospermia is when the absence of spermatozoa is not caused by a defect in the reproductive tract, but it’s because there is no actual sperm production happening.
- Aspermia is the absence of semen, also called anejaculation.
- Cryptozoospermia is a type of low sperm count. Initially, it can be mistaken as azoospermia, but with further tests, it can be ruled out.
- Oligozoospermia is when the semen has a low concentration of spermatozoa.
- Asthenozoospermia is when the sperm has lower motility than the low reference limit.
- Teratozoospermia is the presence of sperm with abnormal morphology in the semen.
- Hypospermia is the low volume of semen (ejaculate).
- Necrozoospermia is when the semen contains very low amounts of alive sperm and high amounts of immotile sperm.
- Sperm DNA fragmentation can be caused by multiple factors such as drug use and exposure to toxic chemicals. Oxidative stress is the number one factor causing DNA fragmentation and degeneration.
- Sperm antibodies in the semen can cause sperm cells to stick to each other, or reduces their motility.
- Immunological infertility is when the semen has anti-sperm antibodies. The body mistakes your own spermatozoa as a foreign object and starts attacking itself.
Testicular Factors
Testicular factors also play a significant part in male fertility. Since spermatogenesis occurs in the testicles, any damage or abnormality to them can cause infertility. These problems can be due to birth defects and genital abnormalities, while others occur later in life. Some testicular factors are possible to prevent. Factors that affect the testicles and spermiogenesis are as follows:
- Previous infections: Untreated STIs can damage the testis, thus affecting spermatozoa quality and production.
- Varicocele: Varicocele is a condition where the veins that are in charge of blood circulation in the scrotum don't work properly. The oxygen-deficient blood starts to pool in the veins, and it depletes the testes of proper nutrition, directly affecting spermatogenesis.
- Congenital & genetic abnormalities: Genetic diseases can cause some abnormalities to the testes where the testes do not descend or grow properly, and lead to infertility.
- Hypogonadism: Gonads are the sex organs that produce sex hormones. In men, the testicles produce testosterone. Hypogonadism is when the testes aren't developed enough to produce spermatozoa or testosterone.
- Hyperprolactinemia: In men, hyperprolactinemia can create hypogonadism-like symptoms and can negatively affect fertility.[1]
- Testicular cancer: The presence of cancerous cells can interfere with testosterone and spermatogenesis. Both the presence of cancer and its treatment can cause infertility.
- Undescended testes: The scrotum holds the testes just far enough from the rest of the body for spermatogenesis to occur. The undescended testes are still in the body, and the body is too warm for sperm production, so the amount of spermatozoa produced is significantly reduced.
- Testicular injury: Severe injury to the testicles can lead to a decrease in sperm production and shrinkage of the testes. In most severe cases, the testicle needs to be removed.
Sperm Canal Problems
Problems with the vas deferens can indicate infertility. Essentially, with vas deferens problems, there is healthy sperm production, but the cells are not present in the ejaculate, or there is no ejaculation because of factors affecting the canal. These problems can present as obstructive azoospermia, where the absence of spermatozoa is due to some malformation of the vas deferens.
- Genetic diseases: Men who carry the genetic mutation for cystic fibrosis have CBAVD, but they have healthy spermatogenesis.
- Congenital Bilateral Vas Deferens Agenesia (CBAVD): This is when the vas deferens is absent since birth. Thus, the spermatozoa cannot leave the epididymis.
- Injury: Vas deferens can get injured during other surgeries or activities.
- Vasectomy: If you had a vasectomy, your vas deferens was cut and sealed, thus spermatozoa cannot exit the epididymis.
- Previous Infections: Untreated STIs can affect the function of vas deferens.
Ejaculation Problems
Problems with ejaculation don't mean that a man is sterile. A man can have completely healthy and normal sperm production but might have problems just with ejaculation. Some of these problems have physiological causes, like ejaculation problems due to radiotherapy, while others have psychological components. If you're having problems with ejaculation due to psychological issues, we want you to know that this is very common, and there is help available. Some of the common ejaculation problems that men deal with are;
- Premature ejaculation: Premature ejaculation can prevent a man from ejaculating into the female reproductive tract and can reduce the chances of fertility.
- Retrograde ejaculation: During retrograde ejaculation, the sperm falls into the bladder instead of being ejaculated.
- Erectile dysfunction: Erectile dysfunction can make intercourse difficult, and can even prevent it from taking place.
- Radiotherapy: Radiotherapy can reduce the amount of semen produced.
Substance Use
Substance use and medications have significant effects on fertility. The misuse of illegal and prescription drugs can alter the way your body and hormones work. For this reason, it's important that you avoid the use of illegal drugs, and do not misuse prescription drugs. You must consult a doctor before you're using any medications, over-the-counter or prescription. You should also avoid the use of natural remedies as the amount of active ingredients can vary from product to product. Some of the most common medications and remedies that can affect male fertility are;
- Sulfasalazine: Used in the treatment of some autoimmune disorders, and prolonged use of sulfasalazine can suppress fertility.[2]
- Anabolic steroids: Human Growth Hormone is necessary for the treatment of hypogonadism-related male infertility. However, for fertile men, the recreational use of HGH and other anabolic steroids can have detrimental effects, ranging from gynecomastia to infertility. [3]
- Chemotherapy: Chemotherapy can damage not only the testes but the germ cells that turn into spermatozoa themselves. For this reason, patients that are about to go through chemotherapy should consider a form of fertility preservation before their treatment begins.
- Herbal medicine: The use of herbal treatments is controversial in all branches of medicine. The effects of herbal medicine are unpredictable and can interfere with sperm production.
- Addictive substances: The use of addictive legal or illegal drugs can affect sperm quality. Oxidative stress from alcohol and nicotine use can damage sperm DNA.
- Medications: Some anti-hypertension drugs, antidepressants, and antibiotics can interfere with your hormones and cause erection problems.
- Exposure to poisonous chemicals: Toxic chemical exposure and oxidative stress due to substance use or environmental factors can lead to sperm DNA fragmentation.
How is male infertility tested?
When it comes to analyzing male fertility, semen analysis is the most important examination, as it gives us an idea about the overall health of the spermatozoa and the reproductive system.
Sometimes, depending on the pathology of the sample provided, adjunct tests might be necessary. Evaluation of vitality is conducted for patients with low motility and can lead to a further diagnosis. The presence of leukocytes is examined, which can indicate infection. The concentration of seminal fructose is examined to see if the patient has obstructive azoospermia if the volume provided was too low.
Semen Analysis: Step by Step
Now that we have learned about the male reproductive system and the causes of male infertility, we can move on to the steps of semen analysis. If you're thinking of getting IVF, you'll have to go through at least 1 or 2 rounds of semen analysis to produce correct data. We know that patients might feel insecure, and have some questions when it comes to the sample collection process. We will go through all the steps of semen analysis so you'll know what to expect and be prepared.[4]
The samples provided are usually compared to the World Health Organization guidelines:
| Liquefaction | 15-30 minutes |
| Semen age | 0-60 minutes |
| Color/appearance | White-gray/opaque |
| Viscosity | Disperse drops (thread should be less than 2 cm long) |
| Volume | 1.5 mL or more |
| pH | 7.2 or higher |
| Total Motiliy (progressive+non-progressive) | 40% or higher |
| Progressive motility | 32% or higher |
| Sperm concentration | 15 million per mL or more |
| Total sperm count | 39 million per ejaculate or more |
| Undifferentiated round cells | Less than 1 million per mL |
| Morphology (normal forms) | 4% or more |
| Vitality | 58% or more |
| Peroxidase-positive leukocytes | Less than 1 million per mL |
| Seminal fructose | 13 μmol per ejaculate or more |
Step 1: Providing a sample
For semen analysis, the male partner has to provide a sample. The most important part of this process is abstinence. To provide the best quality sample, the male partner must abstain from ejaculation (intercourse, masturbation) for at least 2-3 days before the collection. Because of the variability in different samples, you might need to provide 2 different samples 2 to 4 weeks apart for the best analysis.
Step 2: Macroscopic evaluation
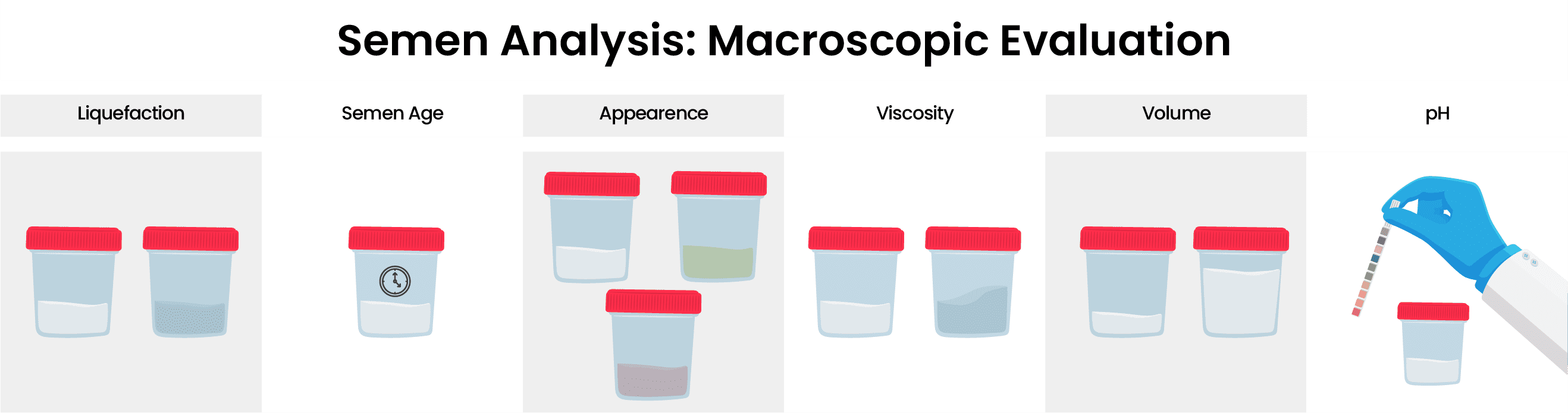
Liquefaction: Liquefaction is when semen goes from a gel-like consistency to a watery consistency because of enzymatic reactions. The time of liquefaction should be around 30 minutes, and if it exceeds this time it can indicate that the sample collection was not complete, abnormality of the prostate, ejaculatory duct obstruction, congenital absence of seminal vesicles, or genital tract infection.
Age: Semen age is how much time has passed since the collection of the sample, and it shouldn’t exceed 60 minutes for analysis.
Appearance: A healthy sample should have a watery consistency and white-gray opaque color after liquefaction. If it appears more transparent, it can indicate low sperm concentration. If there is a presence of blood cells in the semen, it can appear reddish/brow mt-4 mb-4n. If the sample has a yellowish color, it may indicate jaundice, vitamins, drugs, or even the food you eat can affect the color.
Viscosity: Viscosity is determined by aspirating the semen and analyzing the way it drops. Semen hyperviscosity occurs in 12% to 29% percent of patients and it may indicate a problem with the accessory glands. Abnormal viscosity can also indicate a low prostate or seminal vesicle function, or it can indicate an infection of accessory glands when otherwise they’re normal. Hyperviscosity is a serious problem, and it’s associated with low fertilization rates, disrupted embryo development, and pregnancy failure.
Volume: Semen volume is an indication of the health of accessory glands. With age these glands produce less and less secretions, leading to a decrease in the volume. Abstinence is an important factor when it comes to providing a sample with a good volume. A volume less than 1.5 mL is considered abnormal and can indicate a short period of abstinence or an incomplete sample. Ejaculatory duct obstruction, congenital bilateral absence of the vas deferens, and partial retrograde ejaculation can also be the reason for low volume. The complete lack of ejaculate indicates aspermia. If there is a low volume of semen, transrectal ultrasonography is used to examine the seminal vesicles and the ejaculatory duct.
pH: pH is an important factor, and abnormally high pH levels can indicate problems with the accessory glands, incomplete collection of the sample, or an infection. Abnormally low pH levels combined with a low volume, and low sperm count can indicate ejaculatory duct obstruction or congenital bilateral absence of the vas deferens.
Step 3: Microscopic Evaluation
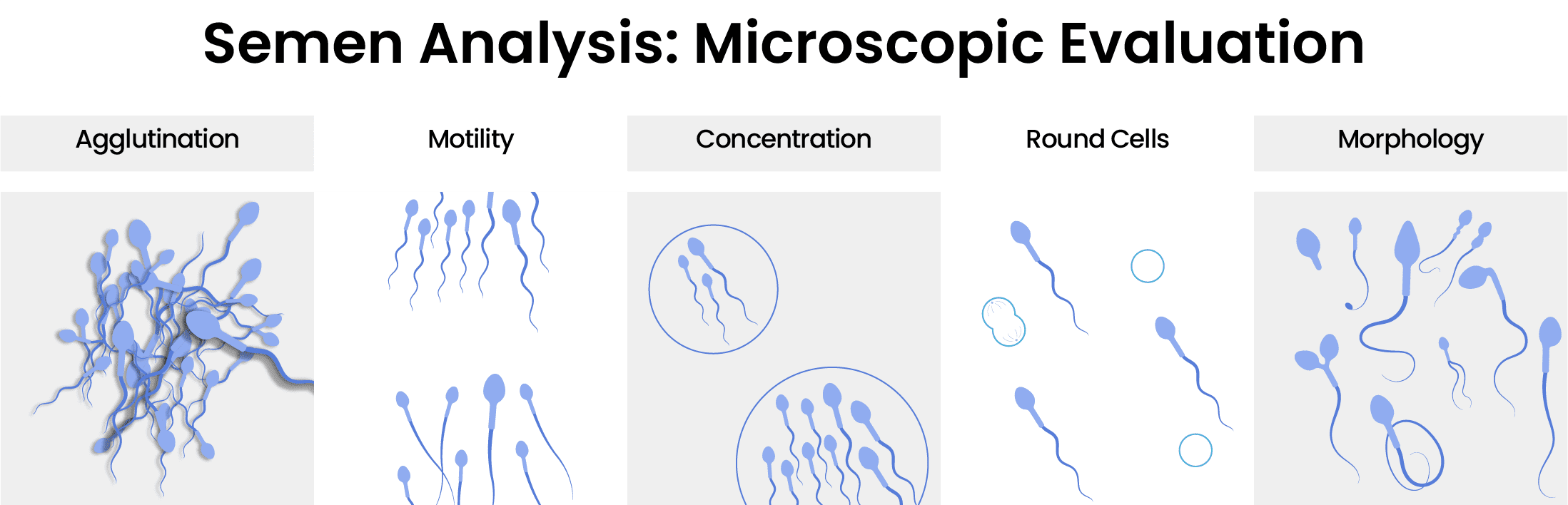
Agglutination: Agglutination is the clumping of moving sperm cells, which is not present in a healthy sample. This clumping can prevent the spermatozoa from moving through the female reproductive tract and fertilizing the egg. If agglutination is present it can indicate the presence of anti-sperm antibodies which can mean the patient has immunological infertility.
Motility: Motility is the movement of the sperm, and it’s one of the most important factors when it comes to fertility. Low sperm motility is diagnosed as asthenozoospermia. Abnormal motility can indicate a problem in sperm morphology or necrozoospermia. The presence of anti-sperm antibodies can also cause low motility, mostly due to agglutination. In rare cases, low motility might be a result of primary ciliary dyskinesia.
Concentration: Sperm concentration is how much sperm the semen has per mL of ejaculate, which should not be confused with sperm count, which is the total number of sperm in the ejaculate. If the sperm concentration is low, the patient is considered oligozoospermic. In addition to low volume, if there is also low pH, and lack of fructose in the sample provided, it can be an indication of obstructive azoospermia, which may lead to further tests for diagnosis.
Presence of undifferentiated round cells: Round cells are immature sperm cells and white blood cells. The abnormally high presence of these cells in the sample can be caused by testicular damage or inflammation.
Morphology: Morphology is also one of the most important aspects of analysis, and the most difficult one. In procedures like IMSI, the spermatozoon with the best morphology is selected for fertilization.
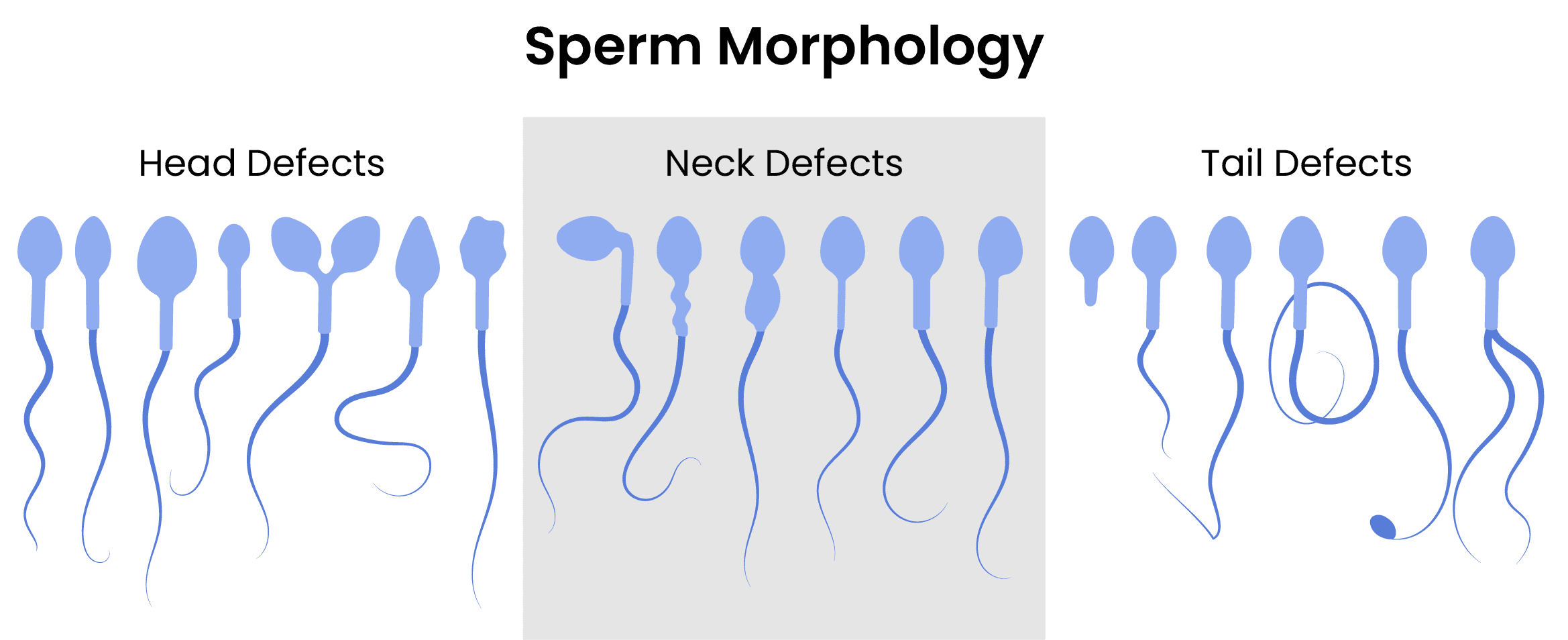
Abnormal sperm morphology is diagnosed as teratozoospermia. Different morphologies can also indicate different diagnoses, but most of the time the reason for morphological anomalies are because of abnormal sperm production, maturation, or genetic diseases. These can cause abnormal spermatozoon morphology, affecting the sperm head, which determines its ability to fertilize the egg. Neck and tail problems affect motility. Most of the time, morphologically abnormal cells can’t fertilize the egg, but if it happens, they’ll likely produce bad-quality embryos.
How does IVF treat male infertility?
For men, IVF treatment focuses on finding a quality spermatozoon that can fertilize the eggs, hopefully resulting in a healthy embryo. Depending on the quality of the semen sample provided, men might have a few different options. IVF samples for fertilization are collected on the same day as the egg retrieval, whether the procedure is surgical or not.
Compared to natural conception, in IVF the semen goes through multiple steps to provide the best sample; the spermatozoa are separated from the semen; leaving anything that can create a complication behind such as round cells, and other secretions, etc.
In situations where the spermatozoa are severely damaged, they wouldn't be able to fertilize the egg on their own. But IVF combined with ICSI or IMSI can be used to fertilize the eggs.
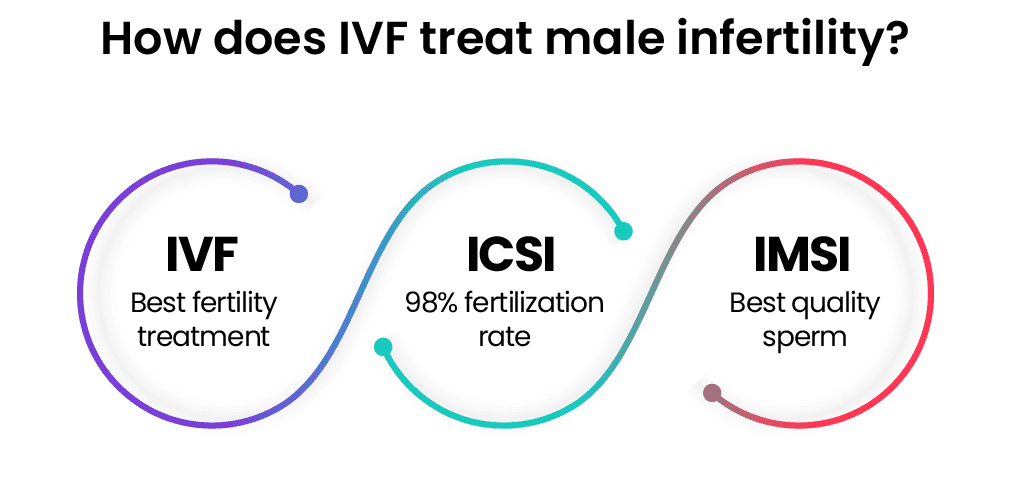
How does ICSI treat male infertility?
ICSI (Intracytoplasmic Sperm Injection) is the best treatment available for male infertility. During ICSI, a single spermatozoon is directly injected into the egg to induce fertilization.
ICSI is used when the sperm quality is very low, or when previous in vitro fertilization attempts proved to be unsuccessful. With just IVF, the chances of fertilization are lower if the sperm concentration is very low. ICSI is not only beneficial for male infertility, but it’s also useful when treating female factor infertility. If the egg quality is poor, ICSI can help with fertilization. Single sperm injection is also very useful when the treatment is conducted with cryopreserved eggs, as they’re harder to fertilize.
With ICSI, men with obstructive azoospermia can obtain consistent fertilization rates. Also, with ICSI, immotile testicular spermatozoa, and even spermatids can be used.
IVF combined with ICSI has a fertilization rate of 98%. There are very few instances where ICSI doesn’t work. In severe cases of non-obstructive azoospermia, sometimes sperm samples can't be obtained. In some cases of globozoospermia, fertilization fails. And not all fertilization can lead to pregnancy as there might be problems with the sperm DNA.
Even though there is some controversy about the use of suboptimal spermatozoa during ICSI, this treatment doesn’t have significant side effects, as most children conceived through ICSI present similar statistics to children conceived normally when it comes to birth weight, NICU admissions, and congenital malformations.[4]
How does IMSI treat male infertility?
IMSI (Intracytoplasmic Morphologically Selected Sperm Injection) is ICSI combined with MSOME (Motile Sperm Organelle Morphology Examination). Essentially, the sperm cells retrieved for ICSI are inspected under highly magnified microscopes that can even see the inner structures of the sperm cells. The morphology of the cells is examined, and the best ones are chosen for injection.
When patients present with severe male infertility, IMSI can be employed to choose the best spermatozoon available. Using sperm that’s morphologically better has better outcomes when it comes to embryo quality. Choosing the best spermatozoon available can also compensate for poor egg quality due to advanced maternal age. [4]
How does IVF work for a man?
IVF can be just as stressful for men as it is for women. However, the IVF process is relatively easy for men. Even though the male partner might not have infertility, we think it's important that they are just as involved in the process, and are there to support their partners.
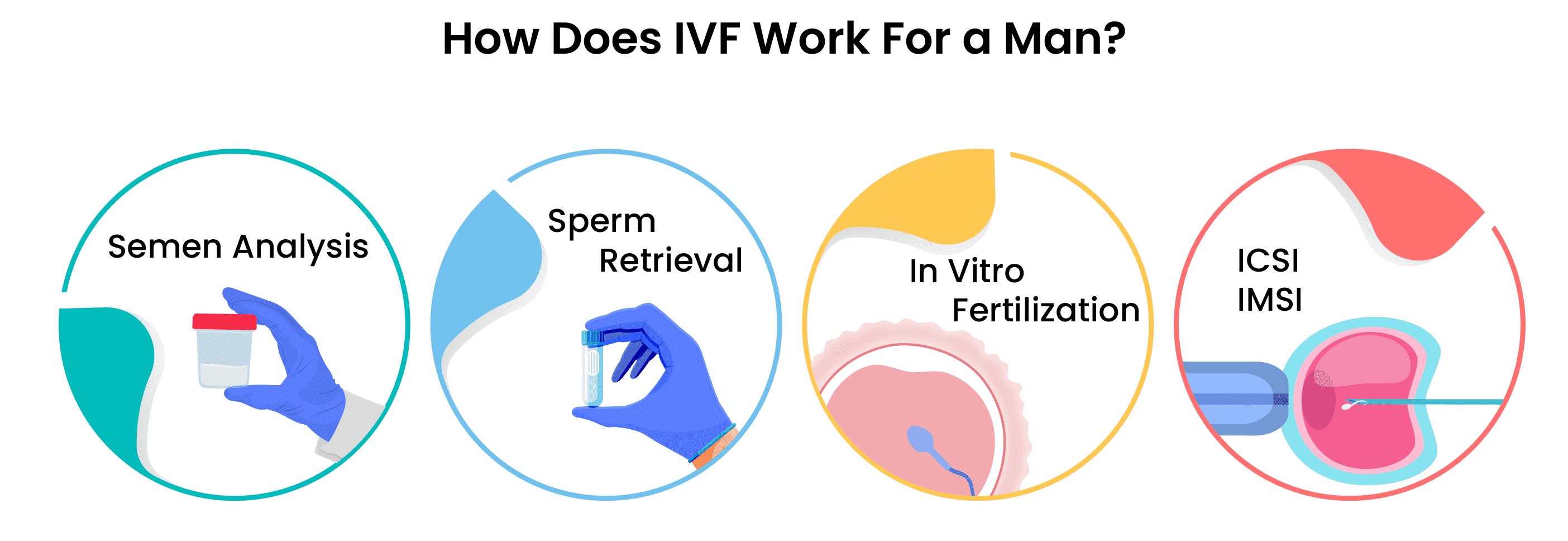
The IVF process for men begins with the semen analysis we talked about above. Depending on the results of the semen analysis, men have a few different options when it comes to treatment.
- If there are enough healthy spermatozoa in the sample, they're washed and left to fertilize the egg in vitro during regular IVF.
- If the sample doesn't have enough spermatozoa, surgical sperm retrieval is used on the day of egg retrieval.
- After surgical sperm retrieval or the ejaculated sample is washed, ICSI is used to fertilize the egg.
- If the infertility is severe, and it's difficult to find a healthy spermatozoon, IMSI is used to choose the best cell.
IVF Sperm Retrieval
If you have no problems with providing an ejaculated sample, and your sample contains enough spermatozoa you won’t be going through any operations. You’ll just have to provide a sample, the same way you did for semen analysis. For patients with insufficient samples, there are procedures available to get the samples needed, which we will talk about further down in this chapter after answering some common questions about the retrieval process.
How is sperm collected for IVF?
If the first semen sample proved to be healthy, on the day of egg retrieval the male patient is asked to provide another sample. Instructions are given to the patient on how to collect the sample in advance. Sperm samples are collected by masturbation in a private and sterile room. The male partner is expected to ejaculate into a sterile plastic cup, without using any lubricants, condoms, or spermicidal agents. The sample then will be sent to the lab for preparation.
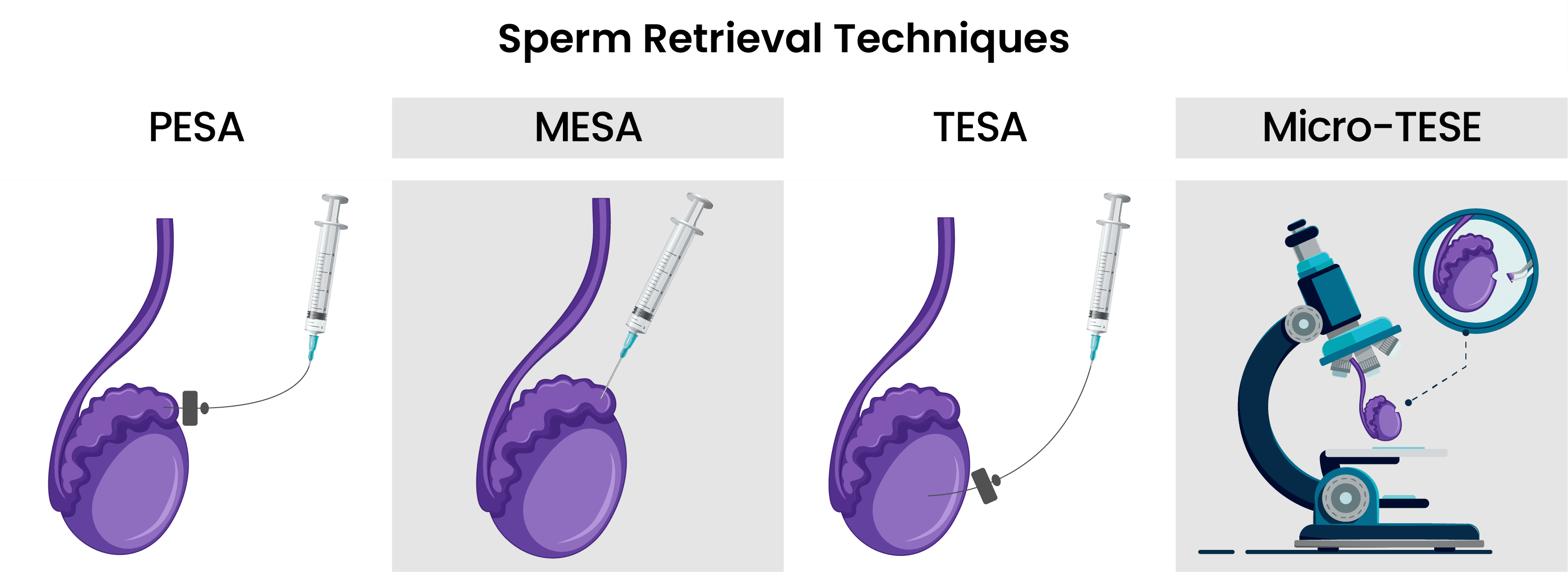
If the sample didn’t prove to be sufficient, or the patient had a vasectomy before, the patient has to go through a sperm retrieval procedure like PESA, MESA, TESA, or Micro-TESE.
How many vials of sperm for IVF?
To make a proper semen analysis and for IVF, it’s expected that the male partner provides at least 1.5 mL of semen.
How old should sperm be for IVF?
Samples should be collected on the same day as egg retrieval. The preparation and waiting time for the sample should not be over an hour. After the sample is prepared, it can be incubated until insemination or cryopreservation.
Minimum sperm count for IVF?
According to WHO (World Health Organization) guidelines, sperm count should be between 39 million and 928 million in the ejaculated sample.
How to get the best sperm sample for IVF?
To get the best sperm sample, please follow your doctor's instructions on how to give the sample, and have at least 2-3 days of abstinence.
How to improve sperm quality for IVF?
To improve sperm quality, you will need to go through some lifestyle changes, like changing your diet and exercise routine. In our guide to IVF preparation, we extensively talk about how you can improve your sperm quality.
Can you do IVF after vasectomy?
Yes, if you have healthy sperm production, you can have IVF combined with ICSI with the help of procedures like PESA.
Sperm Retrieval Techniques
For patients who don’t have sperm cells in their semen, due to some genetic condition, or vasectomy, there are surgical procedures to help them retrieve sperm cells for IVF. All of these procedures are performed under local and intravenous anesthesia, and recovery time is minimal. These procedures are performed on the same day as egg retrieval so that ICSI can be performed as soon as possible.
-
PESA (Percutaneous Epididymal Sperm Aspiration)
PESA is performed on patients with obstructive azoospermia. The samples are collected from the different parts of the epididymis with a syringe until enough motile sperm cells are collected. If enough sperm cells are not retrieved, TESA is performed during the same operation
-
MESA (Microsurgical Epididymal Sperm Aspiration)
During MESA, the skin of the scrotum is cut, and the testis is exposed. The epididymis is cut and the doctor chooses an enlarged tubule for sperm extraction. The fluid inside the tubule is collected. This procedure can be performed in different parts of the epididymis until enough sample is collected. Most of the time, MESA produces enough sperm for ICSI and cryopreservation. However, if the sample retrieved wasn’t enough, TESA or TESE can be performed during the same operation.
-
TESA(Testicular Sperm Aspiration)
TESA is performed under local and intravenous anesthesia. A needle is used to retrieve a small sample of testicular tissue that contains seminiferous tubules. The sample tissue is sent to the lab, where the personnel will extract the sperm from the tissue. If the sample isn’t sufficient, the procedure is performed on the other testis.
-
Micro-TESE (Microdissection Testicular Sperm Extraction)
Micro-TESE is a microsurgical procedure performed under local and intravenous anesthesia. The skin is cut and the testis is exposed. The testis is cut and is examined for the presence of enlarged seminiferous tubules which indicate spermatogenesis. The enlarged tubules are removed. If there are no enlarged tubules, random ones are biopsied. These tubules contain mostly immature sperm cells and germ cells. The sample is washed and examined for motile cells. The motile cells are picked for the use of ICSI.
Now that we have a clear understanding of infertility in both men and women, we can move on to learning about the success rates of IVF.
